As healthcare providers, it has been our priority to encourage and maintain as much “normalcy” as possible while following all guidelines issued to protect our residents from COVID-19 over the last 6 months. We have seen firsthand the impact these regulations have had on our residents, and have used creativity to modify the environment, teach our residents how to utilize technology to speak to their family members, and encourage continued mobility and activity. Even with exhaustive efforts to bridge family communication and daily support and love from staff, depression and loneliness among residents continues to rise.
Recently, the Centers for Medicare and Medicaid Services (CMS) has announced new guidance for long-term care facilities in relation to visitation stating, “we recognize that physical separation from family and other loved ones has taken a physical and emotional toll on residents. Residents may feel socially isolated, leading to increased risk for depression, anxiety, and other expressions of distress. Residents living with cognitive impairment or other disabilities may find visitor restrictions and other ongoing changes related to COVID-19 confusing or upsetting.” While allowing visitation will certainly improve resident morale, CMS has also opened the door to increased social interaction between residents throughout the day.
Deep within this guidance, CMS advises to resume communal activities and dining while adhering to infection prevention recommendations. For example, residents may eat in the same room with social distancing. Group activities may also be facilitated with social distancing among residents and use of appropriate hand hygiene and face covering. Facilities may also be able to offer a variety of activities while taking the necessary precautions. CMS further states that “facilities may not restrict visitation without a reasonable clinical or safety cause.”
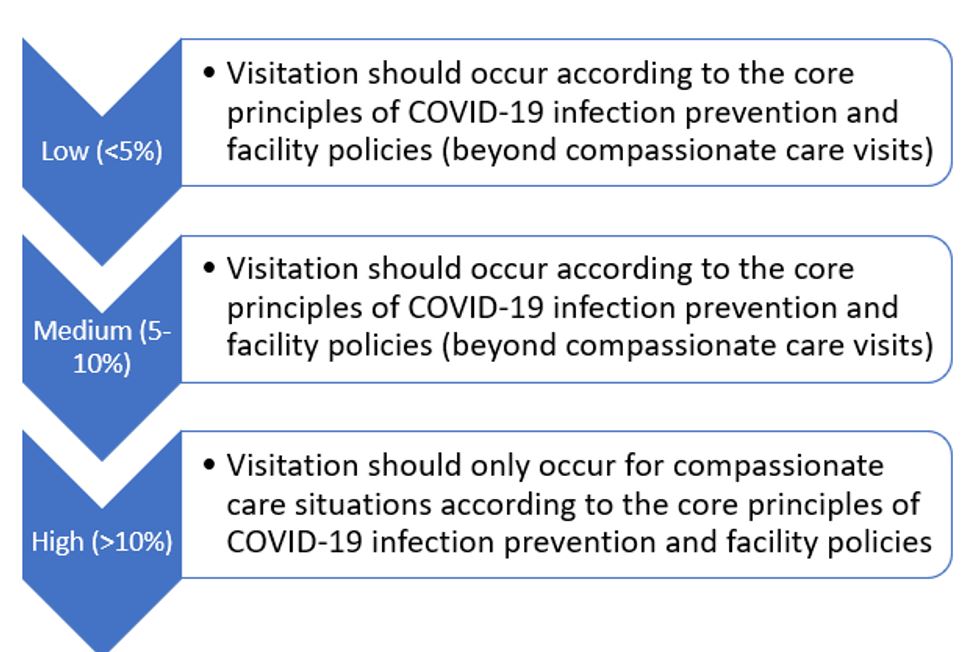
The detailed memo largely outlines visitation for indoor, outdoor, and compassionate care situations. CMS advises that visitation should be person-centered, taking into consideration each resident’s physical, mental, and psychosocial well-being. Outdoor visitation is preferred and should be utilized whenever practicable as it poses a lower risk of transmission. Facilities should also accommodate and support indoor visitation as safety and risk assessment allow utilizing data from the COVID-19 county positivity rate, found on the COVID-19 Nursing Home Data website. Facilities should continue to reduce transmission risk while allowing visitation through the use of physical barriers (i.e. clear Plexiglas dividers or curtains). Among these guidelines, CMS emphasizes the need to follow core principles of COVID-19 infection prevention and use of social distancing.
Although this is not a return to normal, the new guidelines from CMS provide hope for our residents and caregivers by allowing them to have time with their loved ones and other residents within their facility. As healthcare providers, we continue to be the lifeline that can bring awareness to the effects of social isolation on our residents in long-term care. By promoting safe interaction among residents and their families, friends, or neighbors, we are creating a more understanding and supportive environment for our residents.
The CMS guidance for visitation can be found here.
https://www.nationalacademies.org/news/2020/02/health-care-system-underused-in-addressing-social-isolation-loneliness-among-seniors-says-new-report