
Morgan Woods was a high spirited life-of-the-party kind of guy. He was always smiling, loved to dance and was an avid wood worker. Prior to his admit he lived in another SNF and was sent out to the hospital with symptoms of Altered Mental Status. He was treated for bacteremia and toxic metabolic encephalopathy and admitted to our facility to be evaluated by Hospice.
I know all of this because at admit, I spoke at length with his daughter, Temika, as she was really on the fence about either trying therapy or admitting to hospice. I explained the process therapy would follow and she decided to give us a chance, and let us see what we could do to help.
At evaluation, he was bedridden with numerous bed sores, received nutrition via a PEG tube, and was unable to sit up or make purposeful movements. Over the past few weeks, nursing has worked hard to treat his ulcers and they have completely healed. Therapy began with small goals, such as sitting on the side of the bed, reaching out for objects, etc. As therapy progressed this is what we are able to share:
September 6, 2018  He stood in the standing frame for the first time. He fatigued very quickly and would not reach out to engage in any tabletop activity. |

| September 18, 2018 He took his first steps using a rolling walker and the assistance of two therapists. The week prior he took his first steps in the therapy gym with the assistance of three therapists. October 17, 2018 |
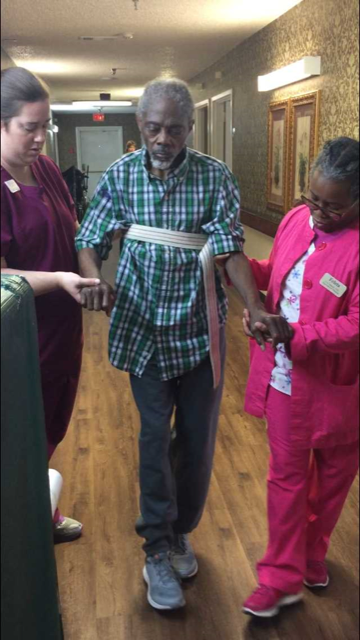 He is now walking down the hallway with no assistive device and hand held assistance of two therapists. |
Morgan has started tapping his feet and dancing in his wheelchair when we play his favorite music like Michael Jackson or Motown. He will reach out to play balloon toss and will flash you the best smile!
During all of this, he took his first bites of food and is now feeding himself and enjoying food daily. Morgan has worked hard and is making wonderful progress. His family is thrilled and so are we!We look forward to seeing him progress even further and one day be able to dance again!

