With the restrictions on visitors, several communities across the country have gotten creative showing appreciation for patients and residents by coordinating “Honk for Hugs” events in a reverse parade fashion.
Forest Hills Care and Rehabilitation, Broken Arrow, OK

The Forest Hills Care and Rehabilitation team in Broken Arrow, OK participated in two community parades, which allowed the patients and residents to see friends and family from a safe distance.
Let’s recognize the team:
Rachel Blanchard DOR
Dianna Sunday PT
Rebecca DeVilliers OTR
Chelsea Holmes OTR
Shannon Pinson SLP
Kelsey Farragher SLP
Saundra Fite PTA
Tara Stephenson PTA
Katie Forler PTA
Candice Ertman PTA
Michelle Kellam COTA
Kimberly Luu COTA
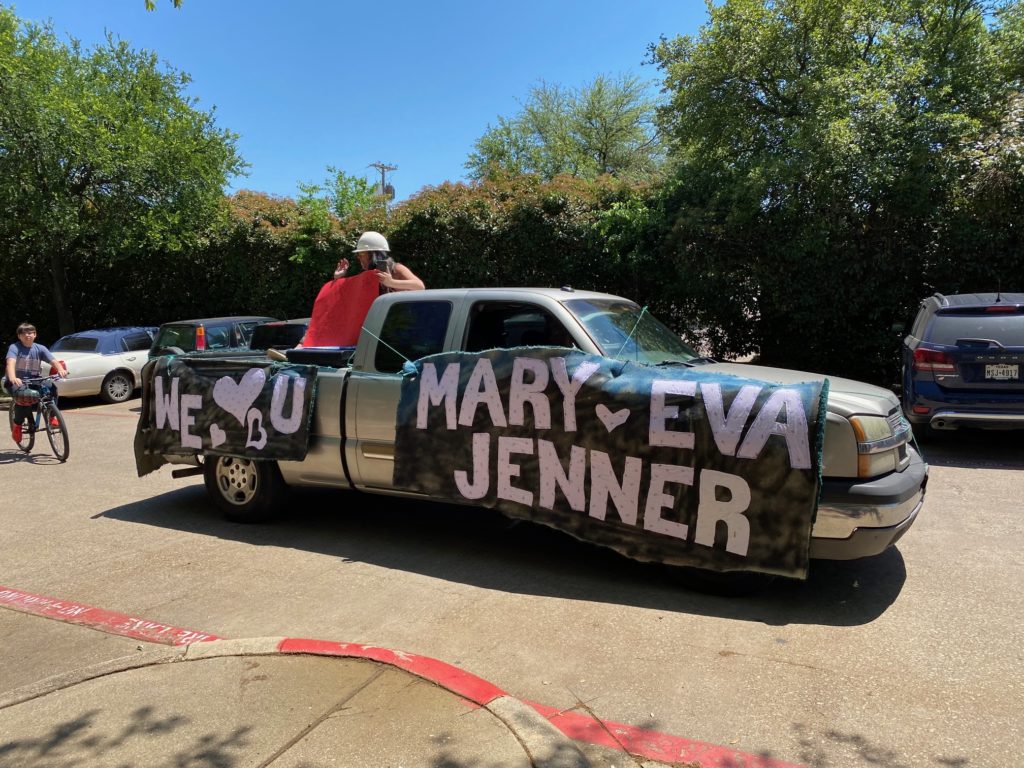
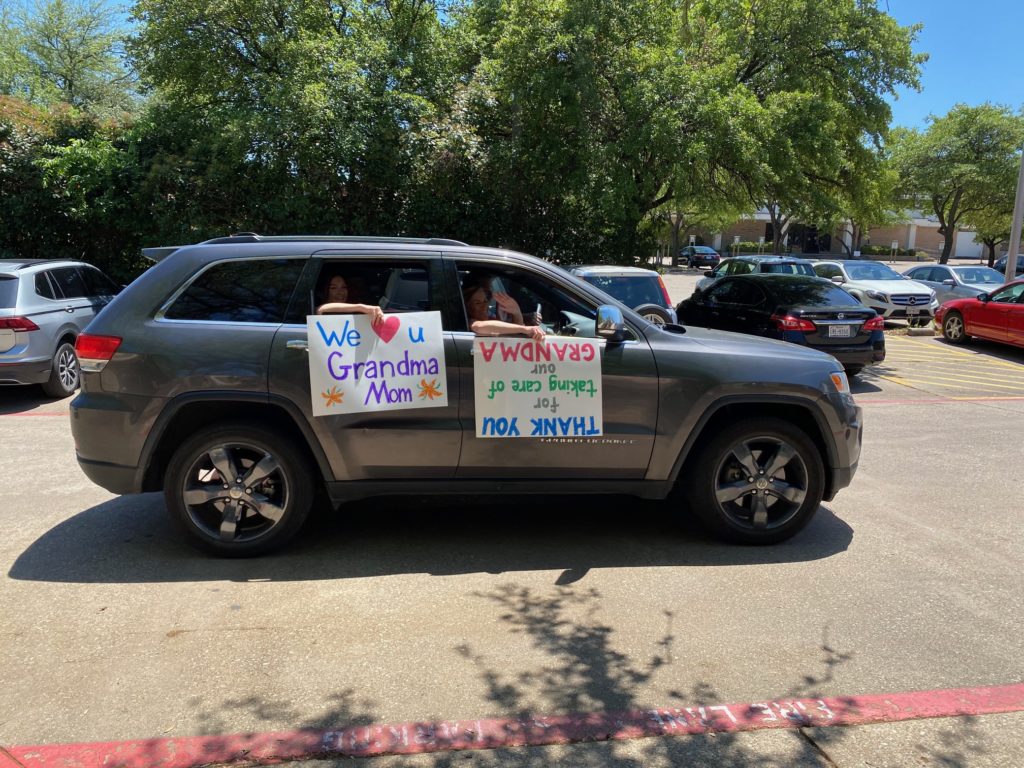
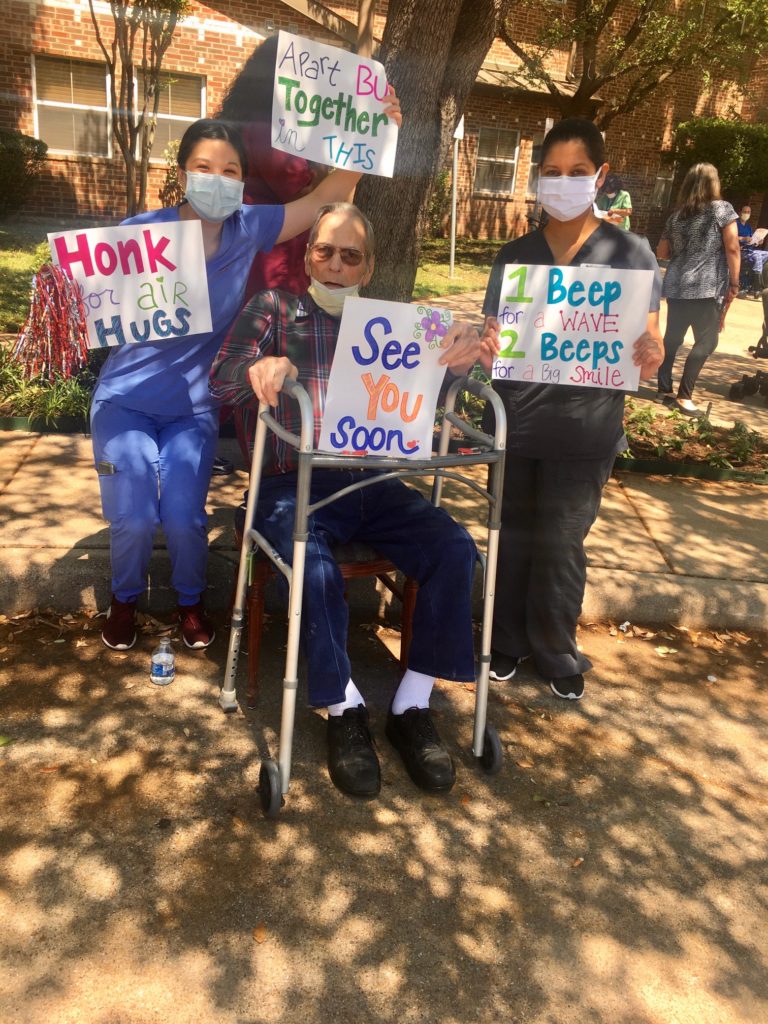
Cottonwood Creek Healthcare Center, Richardson, TX
Cottonwood Creek Healthcare Center in Richardson, TX held a Honk for Hugs event with patients and residents. The patients and residents had so much fun!

CareCore at Westmoreland, Chillicothe, OH
CareCore at Westmoreland’s therapy team in Chillicothe, OH decorated and had patients participate in a “Honk for Hugs” event where the community showed how much they cared for the facility patients and residents.
Let’s recognize the team:
Angie Nartker PT
Kelly Davidson SLP
Crystal Steele PTA
Amanda Karr PTA
Jill Burton COTA
Penelope George PTA/DOR