When the 15% reduction in therapy assistant reimbursement cut was not avoided last fall by Congress, most SNF operators assumed this cut primarily would impact their therapy providers and have little impact on their own bottom line. Pay attention when you open the first 2022 therapy invoice next week. You may be surprised! The assistant cut that began on January 1 is not automatically deducted from the therapy invoice.
That means you may receive less reimbursement while being billed the same amount by your therapy provider UNLESS it was understood that they would make the billing adjustment to reflect the adjusted assistant rates. Otherwise, you may get billed by the therapy company at full fee schedule rates with no Part B Assistant adjustment but get paid at Medicare’s reduced rates.
Many SNF Operators will be forced to make up the difference, but what’s really going on here?
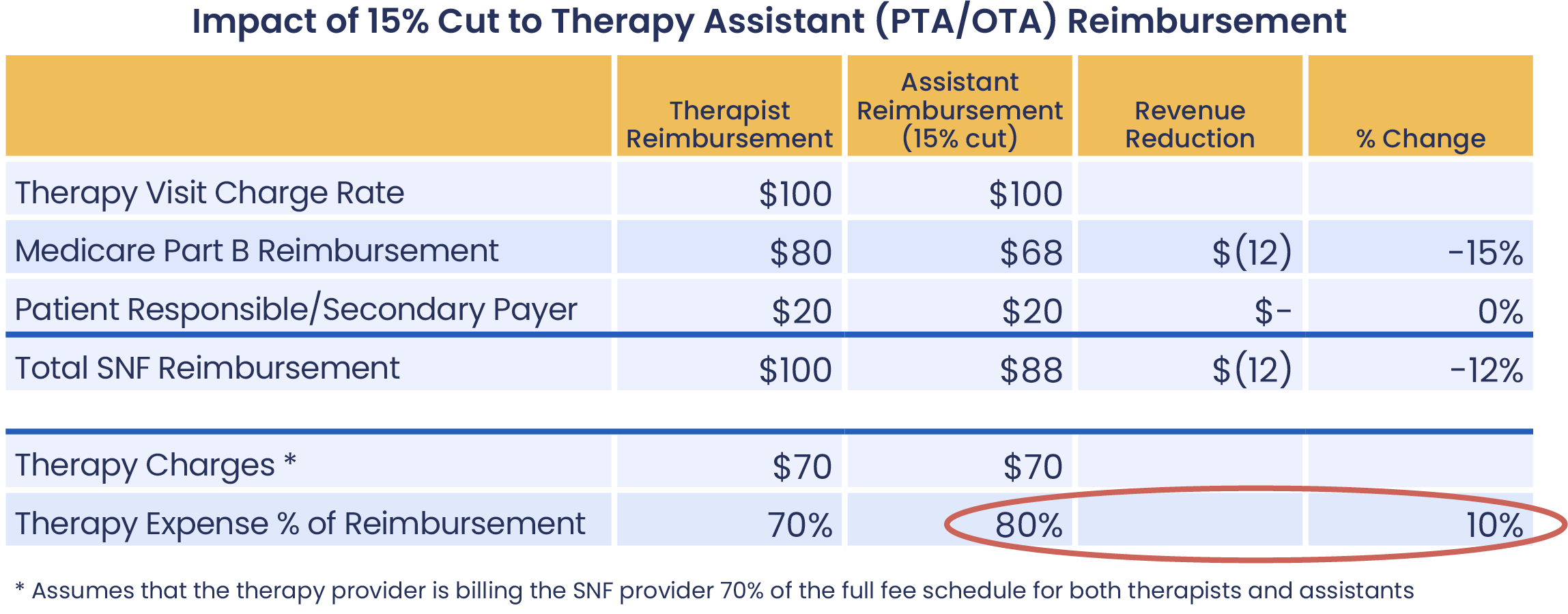
There have been conflicting reports about the actual impact of the 15% reduction in therapy assistant reimbursement, so to clarify, therapy rates are billed 80% to CMS and 20% directly to the patient. The 15% reduction impacts the CMS-billed portion only, so the net reduction to the overall rate is 12%. See the chart below.
By passing the entirety of the rate reduction impact to you, the therapy provider has increased the rates you pay for these assistant services by 10 percentage points!
Therapy Cost Reduction NOT Automatic
Most therapy contracts do not accommodate fluctuations in reimbursement changes from CMS. Traditional therapy contracts bill for a percentage of the currently published Medicare Part B Physician Fee Schedule. If the reimbursement change is directly related to the actual fee schedule – which is often the case – then the therapy invoice will match the reimbursement change. This is not the case with the 2022 assistant cut.
A modifier is added to the billing code to document that an assistant performed the service. This modifier triggers CMS to adjust the reimbursement for that code. In addition, the therapy provider manually must adjust their billing systems to account for these reductions. The process is not automatic. SNF Operators need to check invoices carefully by code and therapist to ensure the bill reflects the reductions.
True Partnership Cost Sharing
Therapy assistants provide skilled care according to the evaluating clinician’s plan of care. In many markets, there are not enough evaluators to meet the needs of all patients, and without assistants, care would be compromised. SNF Operators and their therapy partners need to work together to find ways to retain valuable therapy assistants and continue to achieve strong therapy outcomes while navigating the budget cuts.
In-house Therapy Expense Becomes an Even Bigger Enigma
Managing therapy in-house may seem like insulation against the impact of the therapy assistant cuts. However, many in-house therapy programs already do not have an accurate accounting for the actual cost of their therapy program. Stated otherwise, internal therapy costs per patient easily could exceed average Part B revenue per patient if recruiting costs, staff wages and productivity are not monitored and managed carefully. With increased staffing concerns and rising costs of clinicians, this Part B reduction could swing an in-house program from black to red. The new 15% therapy assistant reimbursement reduction gives in-house therapy operations another reason to take a critical look at their current operations and evaluate the need for a strong external therapy partner who is willing to share risk.
Not having transparency and a complete understanding of how you are being reimbursed and charged for therapy services can have a negative financial impact on your bottom line. As a SNF operator, you know that with razor-thin margins, expense control is critical to the success of your business. Therapy services should not cost more than you are reimbursed. If you would like assistance reviewing your therapy expenses or any additional information, please reach out to us today.
Need help reviewing your current provider invoices?
Copyright © 2024 Reliant Rehabilitation


